Realistic Medicine
On this page
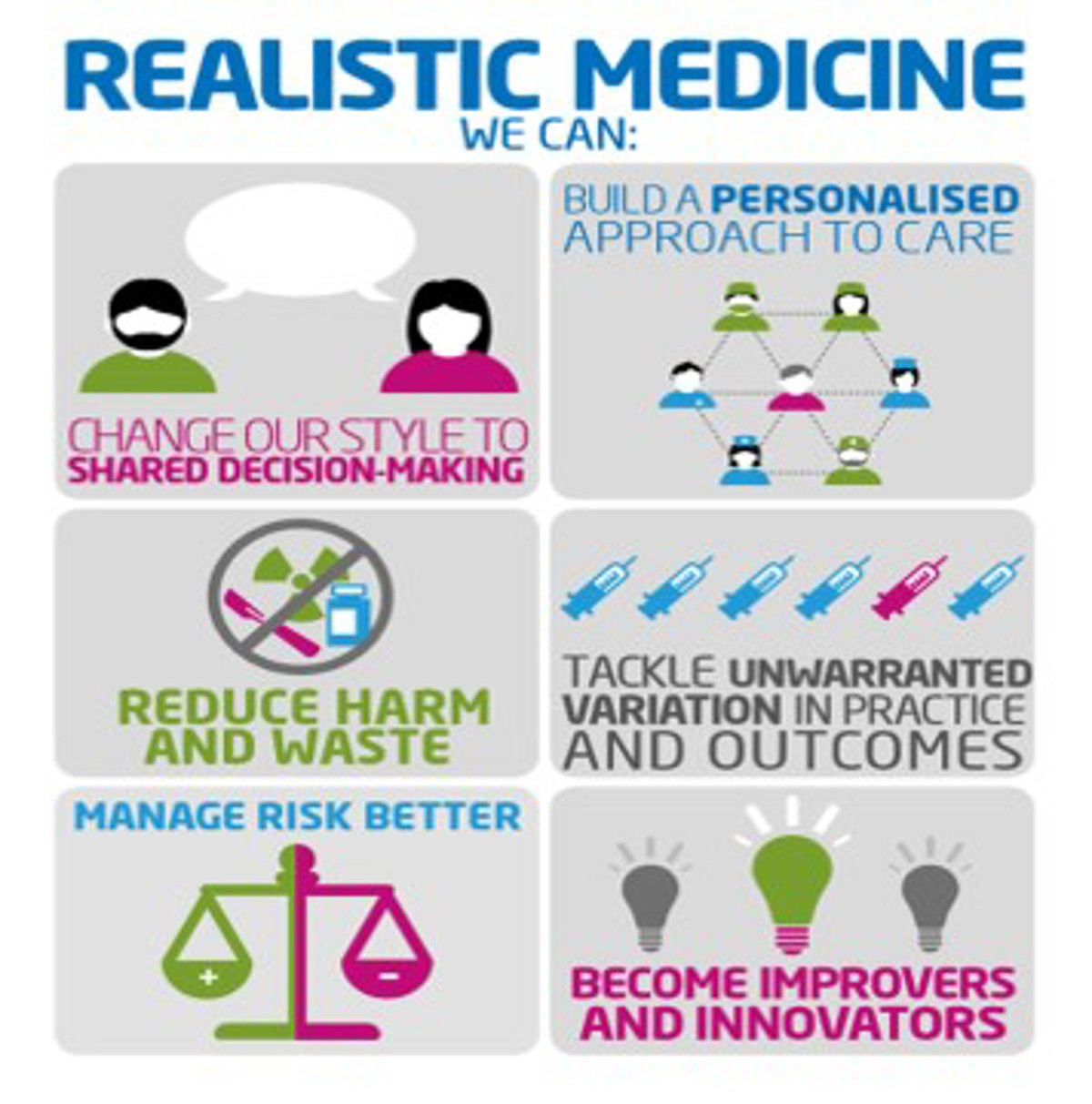
Realistic Medicine is an approach to healthcare that aims to put the patient at the centre of decisions made about their care.
What is Realistic Medicine?
Medical advances have led to people living longer and healthier lives. Living longer can however be associated with complex health and care needs. It is, therefore, more important than ever to have an honest and open dialogue with people about their needs and support them in a way that is helpful to them and their families.
Medical interventions such as drug prescriptions or surgery can have side effects or complications, therefore it is essential that we understand what matters to our patients and ensure the potential benefits outweigh the risks. This requires partnership between care providers and the patients which we refer to as shared decision making.
We must have meaningful conversations with people to plan and agree care in order to base care around what matters most to people, with a shared understanding of what healthcare might realistically contribute. This is the ethos of Realistic Medicine.
How will I benefit from this?
As a patient you will fully understand your healthcare and treatment options, and feel confident and able to have a holistic conversation with your healthcare provider. You should feel empowered to ask questions of your care, have an opportunity for advocacy and good information which you can share with your next of kin.
Introducing Realistic Medicine
Realistic Medicine Introduction from NHS Education for Scotland on Vimeo.
What might Realistic Medicine mean to you?
Healthcare is a partnership between the person receiving care and the team delivering it. In health and social care, there are many treatments that we can offer but it is important that we understand what is most important to you as a patient. For example; If you are a carer for a family member, you may wish to consider treatment options which mean you can continue to care, or be given time to plan for their respite.
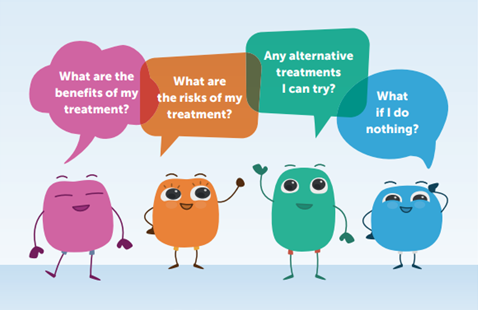
Good quality of life means very different things to different people and Doctors must consider this when explaining the benefits and risks of an intervention such as a medicine prescription or surgery. If you are living with a chronic health condition or are becoming less able to do the day to day tasks which used to be easy for you, then medical procedures or prescriptions can have a greater impact on you and cause more side effects or a longer recovery. This is why it is important that together, we discuss the benefits, risks, alternatives and what you can expect if you don’t proceed with treatment (do nothing).
It is also essential that we consider not only what the NHS can offer in terms of health improvement, but also what an individual can do themselves to improve their health and quality of life. No matter what your level of fitness or ability, there are small changes which we all can make to support our health. As part of this partnership, it is important that we all commit to playing our part in reducing the burden of disease and improving health. Below is a list of resources which can support you in this.
Shared decision making
Realistic Medicine is not about failing to offer treatments; it is about supporting people using healthcare service, and their families to feel empowered to discuss their treatment. That’s why changing our style to sharing decisions with patients is one of our priorities. A move away from “doctor knows best” approach to shared decision making between the professional and patient will require more meaningful discussions about the treatment options available as well as their risks and benefits.
Building a personalised approach to care
Building a more personalised approach to care, in partnership with people through shared decision making, is perhaps the most important aim of Realistic Medicine. We must create a more open and trusting atmosphere that facilitates more meaningful conversations between people and their healthcare professionals that help people make informed choices about their treatment and care options, based on what matters most to them.
Reducing harm and waste
Healthcare professionals are the stewards of healthcare resources. We know that overuse of investigation and treatment can result in harm to patients. By seeking out and eliminating harm and waste, we can provide healthcare that people really value.
There are a number of initiatives underway that aim to help us reduce harm and waste. For example:
Polypharmacy (use of multiple medicines) can be appropriate or inappropriate, and the key healthcare aim for the individual patient is to ensure the safe and effective use of their multiple medicines. Polypharmacy becomes inappropriate when the medication risks begin to outweigh benefits for an individual patient. The aim of addressing this is to identify those patients at greatest risk of harm and to agree a medication regimen that is tailored to their changing needs and expectations.
Tackling unwarranted variation in practice and outcomes
Tackling unwarranted variation is essential to improving outcomes derived from healthcare across NHS Highland. Unwarranted variation is variation in healthcare that cannot be explained by need, or by explicit patient or population preferences. We need to ensure the prevention of harm and waste from overuse and overtreatment, freeing up resources currently used without benefit to clinical outcomes in order to address under-provision of care.
Manage risk better
Realistic Medicine is not about failing to offer treatments. It’s about ensuring decisions are made in partnership with people, helping them to make the choices about their treatment and care that are best for them as individuals. Our view is that more transparency and more meaningful conversations will lead to less litigation, not more.
Become innovators and improvers
To practise Realistic Medicine, we must embrace the best international evidence, employ sound clinical judgment and support empowerment by listening to what matters most to patients. We need to make more effective use of knowledge and skills across the multi-professional knowledge base, and foster the conditions to support innovation in care delivery.
The principles of Realistic Medicine are also being incorporated as a core component of lifelong learning in medical education; in undergraduate and specialty training programmes and through continuing professional development.
Resources
- It's OK to ask about your healthcare
- visit the Realistic Medicine website
- watch videos about Realistic Medicine (at Vimeo)